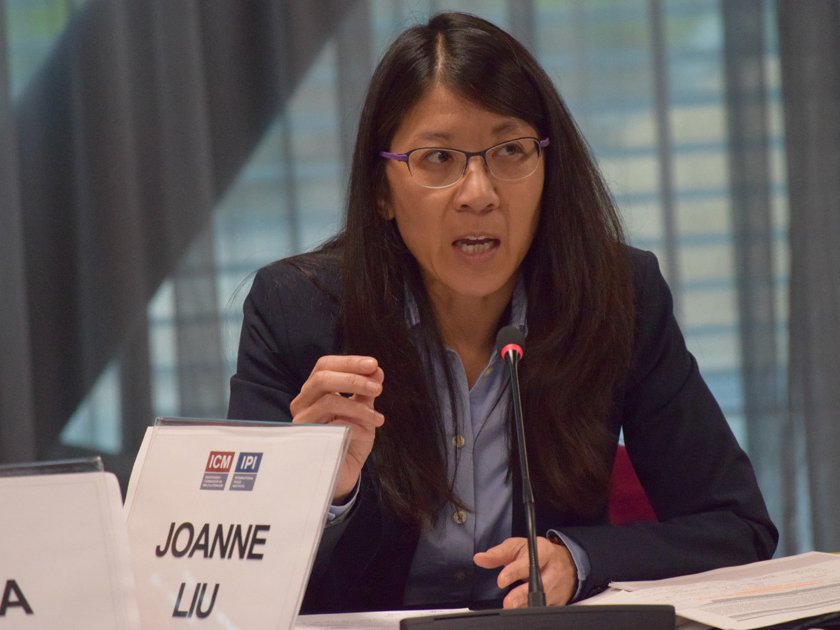
Dr. Joanne Liu, International President of Médecins Sans Frontières (MSF), spoke to Els Debuf of the Independent Commission on Multilateralism about the importance of protecting access to healthcare as well as medical personnel and facilities in war zones, and about ways to address the challenges that arise from delivering healthcare in emergencies. The conversation took place on the margins of ICM’s 13th retreat, on global pandemics and global public health, held on February 8-9th, in Geneva, Switzerland.
This interview has been edited for clarity and length.
You spoke about some of the expectations that one might have of the upcoming World Humanitarian Summit in May and the United Nations Summit on Refugees and Migrants in September. What concrete action do you think—beyond the reaffirmation of basic principles of international humanitarian law—would need to emerge out of summits like these to address some of the concerns you voiced today, with regards to the protection of the wounded and sick, and the healthcare staff who come to their aid in conflict situations?
That is not an easy question to answer. I think from the perspective of a frontline medical humanitarian actor, what we need is a reaffirmation that caring for patients at the front line will not be criminalized; that targeting the medical mission will not be a tactic of war; and making sure that as a doctor, providing medical care for a parties’ enemies will not turn the doctor into an enemy combatant.
In our discussions today, we also spoke about the fact that many of the recent reviews and discussions on global public health do not focus enough on the particular challenges in delivering public health in conflict situations. Do you think there is need for a specific independent panel or other setup to analyze some of these challenges and put forth some specific recommendations?
I must say that after the Ebola epidemic and the number of high-level panels that have been established, and seeing what the output of this has been, I am starting to be a little bit cynical about high-level panels. I do think that we need to address the provision of healthcare services in conflicts, and that is a key issue. The most difficult place to deliver healthcare today remains in conflict areas, but I am not convinced that a high-level panel would make a difference today.
To follow up on that, maybe it shouldn’t be a high-level panel and a very big, formal process. But what about a gathering of people who are working in conflict situations, who have that direct experience? It could be UN agencies, it could be organizations such as MSF, the International Committee of the Red Cross, and others. And also local communities—the front-line responders that are actually doing the major part of the work. Would it be helpful to bring them together to look at specific things, i.e., “these are the things we need to change; these are specific, concrete steps that could be taken”? And then establish a body that could bring it to the attention of states and higher-level UN officials?
The reality today, unfortunately, is that in conflict zones, there are very few actors. We work in Syria, in Yemen, in Afghanistan, and when we look at the “doers” in the field, often we are reduced to a couple of NGOs or organizations. And so, I don’t think it would be a very hard meeting to convene.
That being said, what is clear to me is that we need states. Because the reality today is, who is attacking healthcare facilities? Today we are seeing ourselves facing the fact that four of the five permanent countries of the UN Security Council are part of the coalition bombing hospitals in Syria and Yemen. We need to get—from the UN Security Council—a strong signal that they want to reaffirm that healthcare access would be safeguarded in a war zone; that healthcare facilities, healthcare transport, patients, caretakers, and doctors or other medical staff will not be targeted. That’s what needs to be reaffirmed.
I think that if those rules are not reaffirmed, if this is not clearly stated, we will face some great difficulty and we’re going to have what I call “drifting into total chaos.” I do strongly believe that we have a shared humanity, and I do strongly believe that everybody does understand that when you are in a hospital and you are fighting for your life in the intensive care unit, the last thing you would like to happen to you is to be bombed. And I think we all understand that.
Now we need to live up to that. You spoke during our discussions today of the need to expand on initiatives like Gavi, which is a very efficient public-private global health partnership for vaccinations and immunizations. But it has a problem in that it’s not accessible to middle-income countries who can’t afford some of the vaccines they need—in particular, middle-income countries who have been host countries for refugees, displaced persons, and migrants from conflict zones. So, you said opening up Gavi to middle-income countries would help global public health efforts a significant step forward. What other concrete and easy steps can improve public health prevention and response?
What I was referring to in terms of Gavi is that we have a very simple mechanism that exists, that allows us to get vaccines for highly prevalent infectious diseases to countries who could normally not afford them. And if we were to somehow make the price of Gavi vaccines accessible to middle-income countries that today are struggling because of war, I think it would make a difference.
I think Gavi is a great initiative. I think it should be expanded to countries that are going through really difficult times and are not part of the Gavi list, which are the middle income countries that are at war today. And I think a fair amount of them are in the Middle East, and it would make a difference. All of us are aware now of the children in Madaya, Syria, who would benefit from getting vital vaccines. This is something that we think would be fairly easy, so what we need to do now is to convince the donors of Gavi that we could make a bit of an exception for those countries because that would make a difference in their lives.